Irritable bowel syndrome (IBS) refers to a disruptive colon motility where large intestines are affected, characterized by abdominal bloating, cramps, or pain, and often accompanied with either an increased or reduced frequency in bowel movement and Traditional Chinese Medicine (TCM) has shown to be effective in managing IBS discomforts naturally.
In Singapore, it is surprising to know 1 in 10 suffers from IBS[1], a common functional gastrointestinal disorder affecting especially the younger crowds as we see a rising trend in individuals aged between 20-30. As IBS cannot be definitively diagnosed through standard tests, it is advisable to consider a blood test and stool test to rule out infection and inflammatory bowel disease (IBD), the latter refers to the inflammation or destruction of bowel wall that bring about the narrowing of intestines. Though many individuals may present with mild degree of IBS symptoms, those who have suffered from chronic IBS over a prolonged period experience impaired quality of life as it causes grave disturbance to their daily routine at work or at rest.
Currently, there is no cure for IBS as most conventional medicine is used to manage and relieve the clinical symptoms of IBS.
Common IBS clinical presentation:
- Abdominal discomfort: Abdominal bloating, cramps, or pain – not relieved by flatulence or after bowel movement.
- Changes in appearance and frequency of your bowel movement
Diarrhea – soft, loose, or watery stools, at least 3-5 times a day
Constipation – hard and dry stools, fewer than 3 bowel movement per week - A sensation of incomplete bowel clearance
- Rectal bleeding
- Iron deficiency anemia
- Weight loss
- Feeling depressed and/or anxious in chronic IBS patients
Brain-gut connection
One of the most studied pathophysiology involves the understanding between gut-brain axis (GBA) connection. The brain and gut share a unique intertwined relationship that will impact our physical and emotional well-being through the continuous bidirectional signaling and feedback between the central and enteric nervous system, the limbic system with peripheral intestinal functions[2]. Intensive research has been constantly conducted and studied to understand the complex relationship between brain and the gut as this ensures proper maintenance of our gastrointestinal homeostasis.
When we are stressed, our brain send out signals to the gut via activation of hypothalamus pituitary adrenal (HPA) system to release cortisol from the adrenal gland and prevent effective digestion from taking place as the body initiates the sympathetic system and prepares itself for a fight and defense mode. Henceforth, you may have noticed someone with IBS whom you know is anxious or sensitive, habitually experiences butterfly moments, running to the washroom right before an important interview, presentation, or examination. The intimate relationship between the brain and gut is consequential to our overall gut health system.

Gut microbe changes
There are recent advances to reveal the interaction between intestinal microbiota and GBA through bidirectional channels signaling from the gut-microbiota to brain and from brain to gut-microbiota via neuroendocrine-immune pathway. Alterations of intestinal microbiota such as the presence of small bowel bacterial overgrowth (SIBO) are observed in IBS patients who often experience IBS after intestinal infection or an antibiotics treatment[3].
Traditional Chinese Medicine (TCM) on IBS
From a TCM perspective treating IBS, the interaction between the Shen (mind) and the digestive organs which include the spleen, stomach, intestines, reflects the relationship between brain-gut axis. The Spleen and Stomach are responsible for breaking down and transforming food sources to nutrients for energy uptake and nourishment in the whole body. The small and large intestines control the assimilation of essential nutrients and excretion of waste out of the body.
Spleen deficiency is prevalent syndrome for most IBS patients which include abdomen bloating, pain and/or cramps, loose bowel or constipated and usually feel sluggish or fatigue. Interestingly, spleen is linked to the worry emotion and thoughts in the mind. When one is disturbed mentally or emotionally, e.g., feeling stress, worried, and unsettled, this inevitably results in the discord between Shen and Spleen. The intriguing relationship between Shen and digestive organs is highly demonstrated by studies and observed clinically in IBS patients who present with depression and/or anxiety behavior. Therefore, while attending to improve the Qi and function of the digestive organs, we must take into consideration how to regulate the Shen.
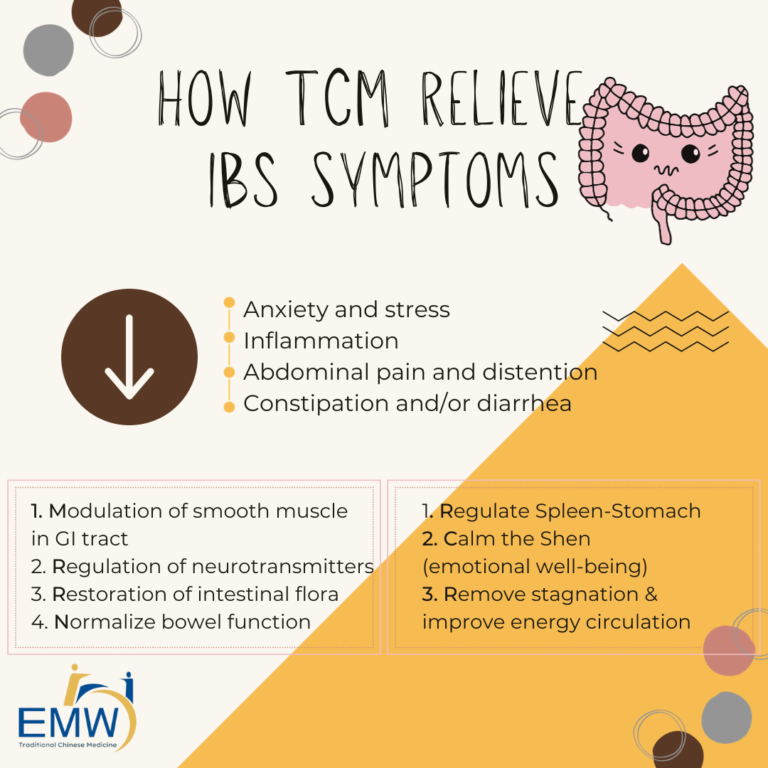
Acupuncture and TCM herbs on IBS
Research has shown that acupuncture in IBS patients stimulates the somatic nervous system and the vagus nerve thereby altering visceral sensation and motility in the intestines [4]. This encourages the parasympathetic system to take place, calms and soothes the spastic intestines while allowing the body to digest, rest and recover.
Besides abdomen bloating, pain associated with alteration in stool frequency and appearances, there are syndrome differentiations to consider in our IBS TCM treatment for acupuncture and Chinese herbal medicine prescription. The most common syndrome differentiations of IBS in a review [5] include stagnation in Liver energy, Spleen deficiency, Spleen-Stomach weakness, Spleen-Kidney Yang deficiency. For example, an IBS patient with Spleen Qi deficiency usually exhibits fatigue, low metabolism, a lack of motivation and constantly overthinking, worrying, and feeling anxious, swollen fat tongue with teeth markings on the side for tongue diagnosis.
Common acupoints used clinically:
1. Bai Hui (GV20)
Location: Rest your thumbs on the tip of your ears for both sides, the intersection point at the crown of your head where both your middle fingers meet
Function: Calm anxiety, clear the mind and lift up the Spirit
Direction: Use your index and middle finger on and massage in circular motion for 1minute. Practice mindful abdominal breathing while massaging this point.
2. Yin Tang (GV29) known as “Hall of impression”
Location: The acupoint between your inner eyebrows
Function: Relieve stress and anxiety
Direction: Use the fleshy portion of your thumb and massage this point in circular motion for 1-2 minutes.
3. Shang Ju Xu (ST37)
Location: Four finger width spacing below Zu San Li (ST36) refer to GERD article, 1 finger width from the anterior border of the tibia, on the outer side of your shin bone
Function: To relieve digestive discomforts involving dampness and heat syndrome, for abdominal bloating, pain, and constipation
Direction: Apply slight pressure using your fingers on this point and massage in circular motion for 2-3 minutes.
4. Tai Chong (LR3)
Location: At the dorsum of the foot, a depression point in between the first and second toes
Function: Resolves stagnation, descends defying energy, calm and soothe anxiety, irritability and anger
Direction: Apply slight pressure using your thumb and massage in circular motion for 2-3 minutes
IBS management at EMW Gut & Moxa Clinic
At EMW, we treat each patient based on syndrome differentiation and design a tailored therapy protocol that caters to individual’s constitution. Treatment plan focuses to relax and calm down spastic colon, improve energy circulation by ensuring smooth flow of Qi and Blood in your digestive organs and remove any heat, dampness, or stagnated energy.
We strive towards enhancing your overall health and wellness to restore your vagus nerve function, for you to feel tranquil and rejuvenated after each treatment session with improvement in digestion and bowel movement.
Your treatment plan will involve:
- Customized TCM herbal prescription for IBS
- Acupuncture
- Moxibustion (for suitable constitution)
- Dietary and lifestyle advice to adhere that will help to reduce recurrence of IBS attacks
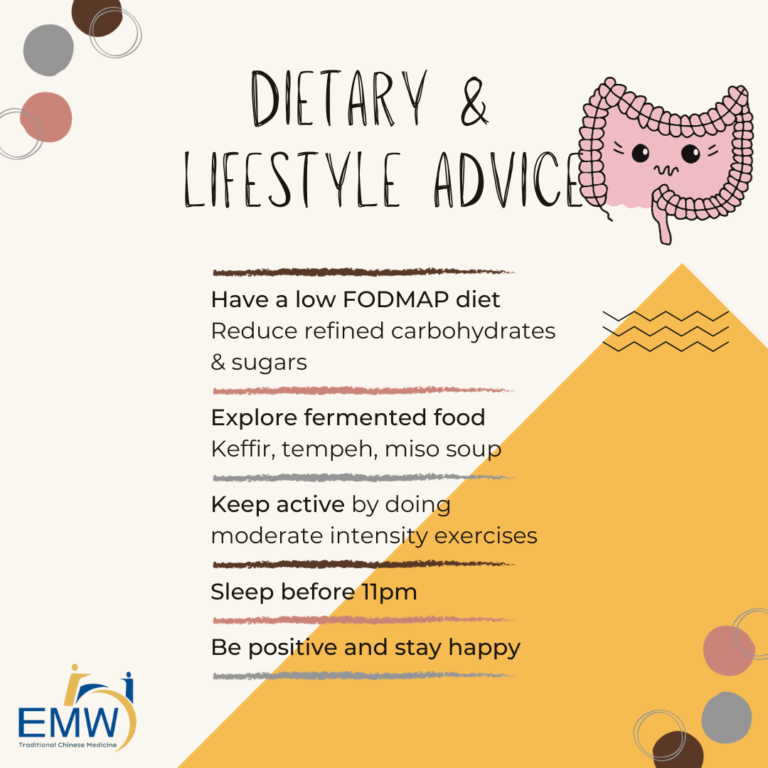
Dietary and lifestyle advice
- Consider low FODMAP (fermentable oligo-, di-, mono-saccharides and polyols) diet, reduce refined carbohydrates and sugars in your meals.
You can include these in your meals:
Diary: kefir, hard cheese, coconut milk
Grains: oats, rice, wholegrains, sourdough, gluten-free bread, and pasta
Proteins: salmon, chicken, eggs, tofu, tempeh
Vegetables and fruits: bean sprouts, bell pepper, carrot, bok choy, potatoes, lettuce, tomatoes, olives, orange, banana, blueberries, grapefruit, kiwi, lemon, strawberries
Nuts and seeds: walnut, almond, macadamia, pine nuts - Be mindful of any food triggers. Avoid food that will aggravate your sensitive intestines.
- Eat smaller meals portion frequently throughout the day (4-5 small meal portion)
- Go for your walks, do light exercises, and practice mindful abdominal breathing to relax and rejuvenate.
- Explore the help from a psychologist if you need to.
Essential oils to reduce abdominal cramps
- Ginger (Zingiber officinale): reduce bloating – 3 drops
- Peppermint (Mentha piperita): relieve abdominal spasms – 2 drops
- Bergamot (Citrus bergamia): support digestion and prevent gas – 2 drops
- Roman Chamomile (Chamaemelum nobile): calm, soothe and sedates – 3 drops
Blend the above essential oils in a 1oz (28g) carrier oil. Apply it on your tummy and massage twice a day in circular motion. Alternatively, you can apply this blend in carrier oil on your foot at the solar plexus area which corresponds to stomach and digestive function.
References:
- Nearly one in 10 Singaporeans suffers from irritable bowel syndrome. Lydia Ng. For healthXchange https://www.healthxchange.sg/digestive-system/irritable-bowel-syndrome/nearly-one-ten-singaporeans-suffers-irritable-bowel-syndrome
- Kennedy PJ, Cryan JF, Dinan TG, Clarke G. Irritable bowel syndrome: a microbiome-gut-brain axis disorder?. World J Gastroenterol. 2014;20(39):14105-14125. doi:10.3748/wjg.v20.i39.14105
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017;11(2):196-208. doi:10.5009/gnl16126
- Effectiveness of acupuncture to treat irritable bowel syndrome: A meta-analysis. Guan-Qun Chao and Shuo Zhang. World J Gastroenterol. 2014 Feb 21; 20(7): 1871–1877. doi: 10.3748/wjg.v20.i7.1871
- The Diagnosis Performance of the TCM Syndromes of Irritable Bowel Syndrome by Gastroenterologists Based on Modified Simple Criteria Compared to TCM Practitioners: A Prospective, Multicenter Preliminary Study. Jun Song, Ling Yang, Shuai Su, Mei-Yu Piao, Bao-Li Li, Lie-Xin Liang, Guo-Wen Zuo, Zhi-Min Tang, Yan-qin Long, Xiāo-Li Chen, Ning Dai, Jian-Ling Mo, Yue Yu, Wen-Yong Yu, Mei Zhang, Rong-Quan Wang, Jing Chen, and Xiao-Hua Hou. Hindawi. Evidence-Based Complementary and Alternative Medicine, Volume 2020 |Article ID 9507674 | https://doi.org/10.1155/2020/9507674
Our Physicians
Principal TCM Physician
- M.Med(TCM Gynaecology)
- B.Sc(Hons) Biomedical Sciences
- Dip. Naturopath
- Ayurvedic Therapist(500hrs)
- Registered TCM Physician (Singapore MOH)
Senior TCM Physician
- M.Med(TCM Acupuncture & Moxibustion)
- B.Sc(Hons) Biomedical Sciences
- Certified Aromatherapist
- Registered TCM Physician (Singapore MOH)
TCM Physician
- M.Med(TCM Gynaecology)
- B.Sc(Hons) Biomedical Sciences
- Registered TCM Physician (Singapore MOH)
TCM Physician
- B.Med(TCM)
- B.Sc(Hons) Biomedical Sciences
- International Board-Certified Lactation Consultant (IBCLC)
- Registered TCM Physician (Singapore MOH)